What is an Audit and what is the difference between an Audit and a QI project?
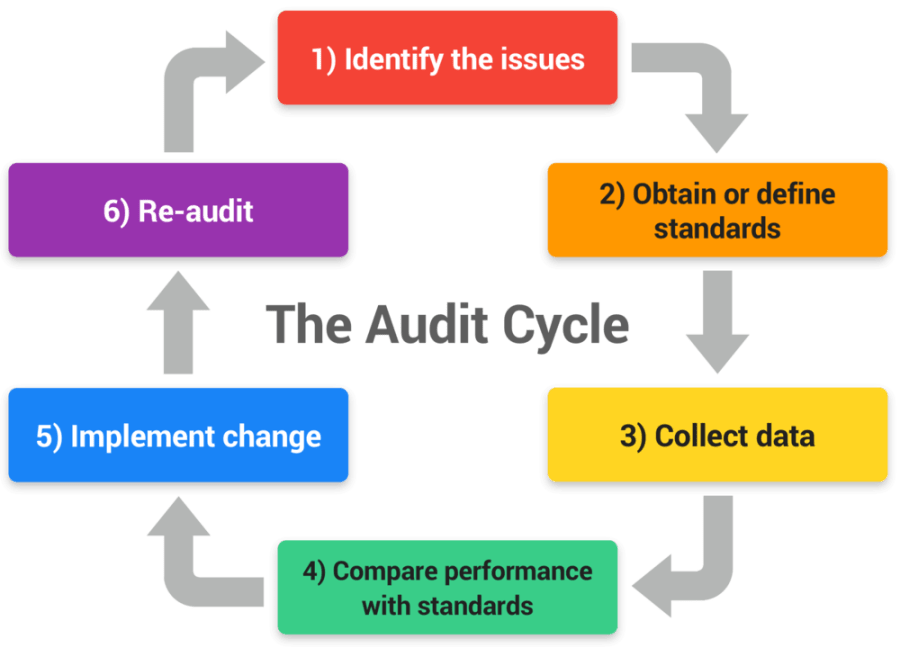
Healthcare professionals are expected to regularly review their clinical practice against the expected standards. Clinical audits are a part of the quality improvement process where you are comparing your practice with already set guidance. Audits are where you as a junior doctor as well as seniors can make a huge impact of the running of health services. Audits are a advancement feature of your knowledge and experience.
Quality improvement is a wider term which may include repeated cycles of audits and making sure the recommendations are followed through to make sustainable improvement to the service.
In simple terms:
- An audit will give you a snapshot of the areas of clinical practice requiring improvement.
- An audit is usually followed by recommendations and suggestions for improvements.
- Re-audit will assess the improvements thus completing the audit cycle and this will create a quality improvement project.
How do I generate an Audit idea?
One way to generate an idea is to look at the current guidelines in your area of practice. The most commonly used guidelines in mental health are
NICE Guidelines
These are available for free and readily available online. NICE has published guidelines on various topics related to mental health covering a wide range of conditions. You can read the guidelines related to your area of work and compare your practice with the recommended guidance.
https://www.nice.org.uk/guidance/conditions-and-diseases/mental-health-and-behavioural-conditions.
These guidelines are extensive but each of them can be broken down into more specific areas of expected practice to create an audit project.
Maudsley Prescribing Guidelines
These are available in a book format which is updated every few years and can be bought online from Amazon. The Maudsley prescribing guidelines provide extensive guidance on Psychiatric medication and their monitoring.
Local Trust Guidelines
These are readily available via your trust intranet and usually found on the relevant trust intranet website.
These may include:
- Various trust procedures and policies (like the admission and discharge process, capacity assessments)
- Prescribing guidance (your trust lead Mental Health pharmacist should be aware of prescribing guidance and are very helpful in gathering your data and offer excellent knowledge with regards to medication enquiries).
- The Mental Health Act which will include various Sections of mental health act and section 17 leave (your local mental health office will have guidance around various aspects the MHA)
Discussions with local Audit department and senior doctors.
Most NHS trust will have an Audit department already involved in various audits and some trust will have an Audit lead within mental health service. You can discuss your interest in Audits with them and may involve yourself in some already ongoing projects.
Examples of Audits and QIP Projects
These ideas are a rough guide to help your thought process so that you can generate your project idea. Before starting any audit, you must discuss with your seniors and supervisor to gain their permission. Your team members may already have experience and previous experience is always invaluable so never hesitate to ask. There may already be an audit waiting to be carried out.
Audits can be employed in a variety of settings. Listed below are a few such settings.
Psychiatry Inpatient / Ward settings:
Audits on the standard of admission clerking and admission procedures:
When a new patient is admitted to a psychiatry ward. There are some expectations and admission protocols that need to be adhered to. They will naturally, vary between hospitals and trusts but you be able to find your local guidance readily.
A few pointers
- Look at the admission protocols and what is expected when a patient is admitted, i.e. a detailed history, a physical examination, bloods and ECGs.
- After establishing the expected practice, define minimally required standards in the set area.
- Pick up a sample of recent admissions, say for example 20-30 patients or a duration of time i.e. 6-12 months.
- Retrospectively, compare the current practice with set standards.
- Identify any shortcoming and make suitable recommendations.
- Share your findings with the stake holders (ward staff, junior and senior doctors)
- Consider and discuss how the process may be improved.
- Implement the changes and re-audit with in a suitable time frame.
An example of audit on admission physical health monitoring requirement.
Audits on ward rounds:
Once you have got the hang of ward round you may look back and think this could be done differently or what if we did this instead of that on a ward round so that it could run more efficiently?
There may not be a set of standards of what is expected in a ward round but you can create a quality improvement project by perhaps understanding the perceptions and expectation of the staff involved.
A few pointers could be to
- Conduct a survey of inpatient nurses and establish their expectations from ward rounds.
- Conduct a survey of doctors to understand their expectations from ward rounds.
- Look at the time taken in the ward round and the roles of other professionals involved.
- Establish the minimum required standards. Are there any minimum standards?
- Retrospectively, look at previous ward entries and documentation to establish how the process of the ward round could be improved.
- Draft your recommendations and share it with your colleagues.
I have seen such project resulting in development of a standard ward round proforma.
An Example
Audits of Medication charts:
Medication involves a large area of our medical practise. You may have heard of significant errors or lack of adequate monitoring in your career so far. You may be thinking how can I improve this? How can my team change our practices to minimize such errors. An audit is an excellent way to tackle these questions. There are several ways to audit medication prescribing.
A few pointers
- Identify the minimum required standards when prescribing medications.
- Look at when a new medication was started. Was it documented in the notes and discussed with the patient? Is the duration specified? Does it require follow up and was this done appropriately?
- Look at the PRN medication charts and check if they are prescribed in accordance with the trust guidelines.
Audits of Rapid Tranquillisation:
Rapid Tranquillisation refers to the use of medication to manage acute behavioural disturbance in order to reduce the immediate risk of harm to the patient themselves and/or others and to reduce agitation and aggression.
Most NHS Trusts have their set policies and guidance relating to rapid tranquillisation. Your local pharmacist again would be an excellent source of information in this area. Rapid Tranquillisation is mostly used in Psychiatry Intensive Care Unit (PICU) settings or General Adult Psychiatry ward settings.
A few pointers
- Find local guidelines/ protocols and algorithms.
- Find the number of cases where rapid tranquillisation was utilised. One way to find cases is to look at incident form data retrospectively. You should be able to find cases where restraint or rapid tranquillisation were used. Is the data following a set guideline?
- Look at the type of medications initiated and how much was given. Was it in concordance with guidelines?
- Compare medication use with the trust guidance.
- Write a report identifying the shortcoming if any.
Audits on Electroconvulsive Therapy (ECT):
There are several different aspects of ECT which can be audited. The ECT process may involve capacity assessment, the Mental Health Act, cognitive testing, documentation of the progress of mood, documentations of the ECT itself.
Each trust usually has set protocols / guidance which are followed before ECT can be given. Here are NICE ECT guidelines.
https://www.nice.org.uk/guidance/ta59/chapter/1-Guidance
Depending on your local guidelines and service needs, you can audit
- Whether the rationale and indications of ECT were discussed and documented.
- If the patient was involved in the discussion and if not, were the reasons documented
- If capacity was assessed using the Mental Capacity Act or if a best interest decision was applied.
- Use of Metal Health Act in relation to the ECT.
- Documentations of the physical fitness, clinical status.
- Documentation of the response to ECT.
- Any recorded adverse effects.
- If cognitive function was monitored
Audits of Section 17 Leave (MHA) :
Section 17 leave is part of the Mental Health Act and there are local guidelines on how to award Section 17 leave and the documentary standards. Your local trust website or the Mental Health Act office should be able to find you the guidance. The MHA office may also keep the record of section paperwork and Section 17 leave forms.
- You can look at the local trust guidelines on Section 17 leave and establish expected standards.
- Retrospectively look at the number of cases and how the forms were completed and whether escorted or unescorted leave was documented in the patients notes or if a time duration was specified. How often hospital leave was reviewed?
- Compare the set standards with current practice and identify shortcomings.
Audits of Discharge Summaries:
There are some basic requirements and guidelines locally on the standards of discharge summaries. You can simply look at the excepted standards and compare it retrospectively with the number of discharge summaries recently completed. It may include
- Diagnosis and ICD 10 codes on discharge summaries
- Medication list and which medications were initiated stopped and why.
- Clearly written follow up arrangements and if those were followed through
- Time taken to complete the summary and copies sent to the GP
If you like to do a larger Quality Improvement Projects involving the quality of discharge summaries. You can
- Start by establishing a mechanism to gather feedback from local GPs on their expectation from discharge summaries.
- Online or paper surveys can be created and sent to local GPs.
- Survey the Senior Psychiatrist around their expectation of what should be included on discharge summaries.
- Look at the already establish standards required for discharge summaries and compare it with the expectations of the GPs and senior Psychiatrists.
- Audit recent discharge summaries from your department.
- You can write a report comparing what GPs are expecting and what we are currently sending or differences of expectations of psychiatrist and GPs on the information given in discharge summaries.
- Draft recommendations to improve standards of the discharge summaries.
Community team / OPD clinic Audits and QIPs:
Letters sent to the GPs – Audit
Letter sent to GPs from a psychiatry clinics can be audited. You can start this project by establishing expectations of the local GPs on what information they find useful on a clinical letter. For example clear documentation of diagnoses, current medication, changes to medication and follow up arrangements.
- You can look at the already established standards of clinical letters within your trust or start by a survey of local GPs and Psychiatrists to establishing their expectations from clinic letters.
- Establish some minimum required standards
- Compare a cohort of clinic letter sent out in the last few months and compare them with expected standards.
An Example of such Audit.
Audit of Non-attendance of OPD / Did not attend appointment (DNA)
Non-attendance to psychiatry clinic appointments can have a significant impact on the service delivery and resources. If the DNA rate is high in your department you can create a QIP based around improving psychiatry clinic attendance rate. This would have a high impact on the delivery of your service and help manage resources on a service provision level.
A few pointers
- Establish the DNA rate of clinics with the help of admin staff. secretaries may have useful information.
- Study the reasons of the DNAs. Is there s common reason for lack of attendance? any particular geographical area? any particular clinic? is transport an issue? are patients getting letters on time?
- Study and discuss the methods to improve the clinic attendance.
- Make recommendations to improve attendance rate using the evidence base.
Systems put in place to send text messages or phone call a few days before the appointment can improve the attendance rate. Many trusts already implement this but other trust may yet to deploy this way of communication.
Physical Health and Metabolic Syndrome monitoring Audit
Certain Mental Health diagnoses and Psychiatry medications are linked with increased risk of metabolic syndrome. Patients with chronic mental health conditions along with long term anti-psychotic medications should be monitored for metabolic syndrome. You may wish to look at this area of mental health.
A few pointers
- You can start this project by reading guidance on the expected standards of physical health monitoring and metabolic syndrome.
- Monitoring criteria may include an ECG, HBA1c, weight, waist circumference and lipid profile
- Find a cohort of patients with chronic mental health conditions and long term use of antipsychotics
- Study the systems in place to monitor their physical health.
- Compare current monitoring with the expected standards.
This is a common audit which I have seen presented in many conferences by junior doctors. You may find yourself in the debate of whose responsibility is to do carry out this monitoring. “Mental health team or the GPs?” Again this in itself can generate a useful QIP!
Audits of Lithium monitoring :
Lithium initiation and monitoring is a frequently audited area. You will find guidance from various sources on monitoring of lithium like NICE, Maudsley prescribing guidelines, and RCPsych. Most trusts will also have local lithium prescribing and monitoring guidelines and your local pharmacist can help you find them.
It is usually easy to find out how many patients in particular team are on lithium.
- Establish expected practices and guidelines
- Collect data retrospectively, on the use of lithium
- Review how often the lithium levels are done and how often bloods are checked for example U&E, TFTs.
- Identify shortcoming and make recommendations.
Audits of Clozapine monitoring:
Clozapine is a frequently used medication for the treatment of resistant schizophrenia especially in general adult psychiatry and forensic psychiatry settings. There is usually a central database that will help you identify the number of patients on clozapine.
You can find clozapine prescribing and monitoring requirement guidelines from NICE, Maudsley Prescribing Guidelines and your local Mental Health Trust Guidelines. Patients on Clozapine also require monitoring of metabolic syndrome markers which you can also use as a standard of an audit.
- Establish expected standards for clozapine prescription and monitoring
- Select a cohort of patients on Clozapine
- Retrospectively look at data comparing current practice with the set standards
High dose (above BNF limit) antipsychotic Audit.
Some patients require higher doses of antipsychotic medication which are above the BNF recommendations. There may be some trust guidelines on how do we monitor these patients and if they require higher level of physical health monitoring. Some GPs maybe reluctant to prescribe outside BNF guidance and may well prefer to keep the patient monitored under secondary care.
Risperidone and serum Prolactin audit:
Risperidone as an antipsychotic is known to increase the serum prolactin level and increased prolactin levels can make patients symptomatic and have short and long term effects on their bodies.
A few pointers
- Find local or national guidelines on the monitoring of prolactin in mental health patients
- Identify patients on risperidone (short or long term) may be with the help of local mental health pharmacist or community team.
- Audit the current practice with expected standards and identify shortcomings.
Audit the Provision of Psychotherapy:
There is an evidence base and guidelines from NICE regarding the importance of psychological therapies in managing common mental health conditions like anxiety and depression.
You can re-familiarise yourselves with the NICE depression treatment guidelines here
https://www.nice.org.uk/guidance/cg90/chapter/1-Guidance#stepped-care
However, the provision and availability of psychotherapy varies across the UK.
You can
- Establish what form of common psychological therapies are recommended for certain mental health conditions by established guidelines.
- Study what therapies are available locally for your patients and typical waiting times.
- Make suggestions to how access to psychological therapies could be improved.
Old Age Psychiatry:
Dementia related Audits and QIPs:
NICE has published detailed guidance on the diagnosis, management and treatment of dementia. Click on the link for current NICE guidance.
https://www.nice.org.uk/guidance/ng97
Different aspects of this guidance can be audited and compared with current practice. The recommendations from this guidance is divided into the following sub-headings.
- Assessment and diagnosis
- Involving people living with dementia in decisions about their care
- Interventions to promote cognition, independence and wellbeing
- Pharmacological interventions
- Managing non-cognitive symptoms
- Supporting carers
- Staff training and education
You could do a quality improvement project in helping to improve the assessment and diagnosis process.
A few pointers may be
- Look at the process of assessment of cognitive impairment
- Time taken from first referral to diagnoses
- Reasons for delay in the process
- Cognitive testing used and the investigations carried out in the process
- Identifying the areas causing a delay in the diagnosis process
- Improve the flow of patients through the service.
Medications prescribed in Dementia:
- Study the local prescribing guidance and the expected standards of dementia medication and their monitoring.
- Review a cohort of cases from the memory clinics retrospectively.
Here is an example of a service audit on supporting carers in dementia by a junior doctor.
Driving and Dementia – Audit
Dementia can affect a person’s ability to drive. Assessing if a patient is driving a car at the initial assessment phase is common practice.
Here are DVLA guidance with Dementia and Driving:
A few pointers may be:
- A study of issues relating to dementia and driving including the (Driving Vehicles Licensing Agency) DVLA guidance. (LINK)
- To establish minimal required standards for the assessment.
- You can study how issues of driving are dealt within the local memory assessment service.
- Check notes say for example, if driving status was asked and recorded in notes. This can be done retrospectively.
- If the patient was driving, what advice was given?
Audits of Inpatients Falls:
Inpatient falls can have a detrimental effect on patients and reduction of inpatient falls is always high on the agenda. A good quality improvement project can be created based on the assessment and reduction of falls. You may look to:
- Identify fall events using the incident reporting and Datix and incident reporting data.
- Look at the pattern of falls, location, timing and outcome
- Study any obvious patterns or particular wards presenting with high number of falls.
- Study the fall prevention strategies and how they can be implemented on a particular ward.
- Discuss your findings with the multi-disciplinary team, ward managers and seniors.
- Draft recommendation on falls prevention.
Here is an example of an inpatient falls prevention project.
A simpler version of an inpatient falls audit may include studying if the falls protocol and local guidance were adhered to following the falls. For example, local guidelines may include a doctor’s review following the fall, a CT head and neuro-observations.
Audit of the DNACPR ( Do Not Attempt Resuscitation ) Audit:
Most NHS trust will have DNACPR policy in place and DNACPR is used frequently on the dementia assessment wards.
- Look at the local DNACPR guidance usually available on the Trust intranet online.
- Retrospectively, check DNACPR decisions if they followed the procedure
- For example, if they were documented and discussed with the family where appropriate.
- Identify shortcoming and make recommendations
An example:
Audit of Venous thromboembolism risk management (VTE):
Elderly frail patients may have their mobility compromised putting them at higher risk of VTE. It would be worth familiarising yourselves with the latest NICE for VTE.
https://www.nice.org.uk/guidance/ng89
Most NHS trust will also have internal guidelines to follow on old age psychiatry wards. You may wish to:
- Identify a cohort of patients on the old age psychiatry ward at risk of VTE.
- Identify how the risk of VTE was assessed and how it was documented.
- What measures and treatments were put in place where risks were identified.
- Compare the current practice with expected standards and identify shortcomings
An example
Audit of Care home reviews of antipsychotic medication prescription for dementia patients
Regular reviews of anti-psychotic medications prescribed for patients with dementia is advised and long term use of anti-psychotics medications in dementia can be harmful. You can
- Look at the guidelines around use of antipsychotics in dementia.
- Standards expected for monitoring and reviews in care homes.
- Study the current practice and systems put in place for monitoring.
- Compare the current practice with expected standards.
Audit of the Management of Behavioural and psychological symptoms (BPSDs) of Dementia
Management of BPSDs can be a major challenge on the dementia assessment ward and dementia care homes. Guidelines are available via NICE Dementia guidelines and the Maudsley Prescribing Guidelines around management of such behavioural symptoms of dementia of and these can be used to audit the current practice.
You can
- Study which guidelines (local or national) are followed locally in the management of BPSDs
- Look at how BPSDs are recorded in patients’ notes,
- What non-pharmacological and pharmacological options are available and put in place.
- Compare the current practice with the expected standards.
Child and Adolescent Mental Health Services (CAMHS)
Audit of ADHD assessment, medication and monitoring requirements
If you are working with CAMHS, you are likely to encounter ADHD clinics.
NICE has published extensive guidance on the assessment, treatment and monitoring requirements of ADHD medication.
https://www.nice.org.uk/guidance/ng87/chapter/Recommendations#medication
Different aspects of these guidelines can be used to create an audit project depending on the service structure, needs and requirements.
Here are a few examples
Learning Disability (LD) Psychiatry
Audit of Epilepsy management in the LD patients :
Patients with learning disabilities (LD) are more likely to develop epilepsy. Specific NICE guidance is available on how to manage epilepsy in patients with LD.
- You can consider looking at the current provision and systems put in place to help and monitor LD patients with epilepsy.
- Identify standards expected from the mental health services.
- Identify a cohort of patients and retrospectively look at notes to audit standards
Using STOMP (Stopping over medication of people with a learning disability, autism or both) project to help audit the service:
You can read more about STOMP here
https://www.england.nhs.uk/learning-disabilities/improving-health/stomp/
After identifying service need for this project you can discuss how to approach this subject with the services you are working in.
You can start by looking at the Challenging behaviour and learning disabilities NICE guidelines
https://www.nice.org.uk/guidance/ng11
Study the pattern of anti-psychotic prescriptions and compare it with the guidance provided by NICE. This can create a good audit.
You can take it to the next level and you can develop this project into a QIP with an aim to reduce the prescription of anti-psychotics in LD patients.
Audit of Hospital Passports :
Healthcare or hospital passport is a document with information about patient with LD and their healthcare needs. It may contain useful information, such as their interests, likes, dislikes and preferred method of communication.
You can
- Audit if hospital passports are used in your service.
- What information is needed on the passports.
- If patients have up-to-date information.
- How often these passports are reviewed and updated.
Psychiatry related Audits if you are working in other medical specialities
Some junior doctors may not be working in psychiatry but interested in applying for Psychiatry training and would like to improve their portfolio by showing they have done a Psychiatry related audit. You can easily do a psychiatry related audit in a general medical setting, surgical ward or the A&E. Here are some ideas:
Audit / QIP on the management of delirium.
NICE has produced comprehensive guidance on the prevention, diagnosis and management of delirium.
https://www.nice.org.uk/guidance/cg103
Delirium is one of the most common presentations in acutely unwell elderly patients on surgical, medical or A&E. You can
- Look at how delirium is identified and recorded in notes.
- The pharmacological and non pharmacological management of delirium
- What delirium reduction strategies are in place.
- Staff training in recognising and treating delirium.
Cognitive tests used on the wards – Audit
You will find situations involving elderly patients on medical wards where their memory and cognition will be questioned such as if the patient has pre-existing dementia or acute confusion with delirium. This is more common in Care of Elderly medical wards.
You can
- Look at what tools (cognitive tests) are commonly used to assess cognition.
- Their reliability and validity given the situation.
- How deficits in cognition are documented and investigated.
Here is a guide recommending assessment of cognition in different settings.
Mental Capacity Assessments and their documentations
Mental Capacity assessments are now part of routine medical work and decision specific capacity assessments and best interest meetings are happening in all medical settings. Most hospitals will have their internal guidance and / or forms relating to capacity assessment and the best interest process.
You can
- Look at the standards expected from the capacity assessment process.
- Documentation of the capacity assessment and best interest decisions.
- Compare the data gathered retrospectively with the expected standards and suggest improvements.
Here are NICE guidance relating to capacity assessment.
https://www.nice.org.uk/guidance/ng108/chapter/Recommendations
Audits of Referral to Psychiatry liaison teams and their outcomes.
Psychiatry liaison teams support medical areas including A&E, medical / surgical wards. The process of referral and expectations may differ depending on where you are working. You can create a quality improvement project based around the interactions of medical and psychiatry teams.
For example:
- Study the referral process between medical and psychiatry team. Is there a form or phone call involved?
- Conduct a survey of the staff regarding their expectations of the referral process. Ask mental health staff what they expect at the point of referral and ask medical staff what are their expectations are from the psychiatry teams.
- Retrospectively, examine data from past referrals such as the indication for the referral, what information was provided? The time taken from referral to assessment, what was expected from both teams and what was the outcome?
- Analysing the data from past referrals and survey of expectations, you may come up with a way to improve communications and referral procedures.
Management of Behavioural and Psychological symptoms of Dementia (BPSDs) on the medical wards
Behavioural and psychological symptoms of dementia (BPSDs) are common with advancing dementia and you will find patients with establish diagnosis of dementia on the general medical wards presenting with agitation, wandering, and aggression.
You can use NICE guidance as a tool to help you develop an audit or QIP.
https://www.nice.org.uk/guidance/ng97/chapter/Recommendations#managing-non-cognitive-symptoms
- Retrospectively, look at how BPSDs were recorded and managed.
- Compare current practice with NICE guidelines
- Identify shortcomings and make recommendations.
- Retrospectively, look at how BPSDs were recorded and managed.
- Compare current practice with NICE guidelines
- Identify shortcomings and make recommendations.
How and where can I present my Audit / QIP?
As audits are generally part of the service improvement exercise, you should present your findings to the teams and clinicians concerned. Consider the stakeholders who would be interested in knowing about your project. This will generally include the people directly affected by the project. Stake holders may be
- Junior doctors, middle grade and senior doctors
- Nursing and other healthcare staff
- Nursing and healthcare managers
You can present your audit / QIP to:
- Local Post graduate teaching sessions.
- Management meetings where stakeholders are present.
- Quality improvement workshops and audit meetings within your NHS organisations.
- Local and national conferences as posters.
Most RCPsych conferences including the Intentional Congress of Psychiatrist accepts quality improvement projects and audits as posters.
How do I include my Audit in my portfolio?
- Power point slides showcasing the main findings.
- A short audit report or abstract.
- Poster of the audit.
Audit abstract or poster will usually have these headlines
- Aims and Objectives
- Background
- Methods
- Results
- Recommendations / Discussions.
Poster designs and templates can be downloaded from the link below. You can make posters in PowerPoint and save them as PDF.
Several other designs are freely available online
Some more examples of completed audits
Further reading:
https://www.rcpsych.ac.uk/improving-care/ccqi/national-clinical-audits